Key Takeaways
- India recorded 1.4 million new cancer cases and 916,000 deaths in 2022. Every Indian has a 10.6% lifetime risk of developing cancer.1
- Early-stage cancer detection dramatically improves survival rates. Stage 1 breast cancer has a near 100% five-year survival rate; Stage 3 drops to 72%.2
- Prostate cancer cases in India are rising sharply, yet 42.9% are diagnosed with distant metastasis compared to just 8% in the USA—largely due to delayed screening.3
- In India’s healthcare system, where treatment delays are common, early detection is not just beneficial—it is essential for survival.
- Organizations that implement preventive screening programs see measurable outcomes: lives saved, lower claims, and higher employee satisfaction.9
{{divider}}
"It's probably just a lump."
That's what my friend and I kept telling each other. We read the statistics together—a certain percentage of lumps are benign. She'd be part of those stats. Of course she would.
Except she wasn't.
Triple negative breast cancer, an aggressive form that doesn't respond to standard hormone treatments. The diagnosis came fast—just weeks after she found the lump. Stage 3.
You know how you read about 1.4 million cancer cases in India, or that 10.6% lifetime risk, and it stays abstract? Just numbers on a page. It happens to other people.
And then it happens to someone you know.
Suddenly you're not reading statistics. You're sitting with them while they try to process words like "aggressive" and "chemotherapy" and "treatment plan." You're the one googling survival rates at 2 AM (her doctor advised us against this). You're watching someone's life split into before and after.
My friend caught it on time. Treatment started immediately. But "on time" shouldn't mean "before it spread too far." On time should mean Stage 1, when survival rates approach 100%. Or earlier—catching warning signs before aggressive cancers ever develop.
My friend's experience isn't unique—it's part of a pattern.
This article examines three different cancer stories to reveal one truth: in India, detection timing determines survival.
Whether it's breast cancer found through self-examination, kidney cancer caught in routine screening, or prostate cancer diagnosed after symptoms appear, the principle remains constant.
Early detection saves lives. Late detection costs them.
This National Cancer Awareness Day and Movember, India's 1.4 million annual cancer cases demand we talk about more than one disease. Breast cancer kills because of late detection. Prostate cancer kills because of late detection. Kidney cancer kills because of late detection.
For most Indians, early detection faces systemic barriers: waiting lists for specialists, delays in diagnostic tests, fragmented care during the most stressful time imaginable, treatment delays stretching from weeks to months, and financial barriers that postpone care even further.
According to the latest GLOBOCAN 2022 report, India recorded 1,413,316 new cancer cases and 916,827 cancer deaths in a single year. Every Indian has a 10.6% cumulative risk of developing cancer before age 75.
Behind each number is someone like my friend. Someone's colleague. Someone's family member. A life that could be saved through early detection.
{{divider}}
India's Cancer Landscape: The Numbers Behind the Crisis
In 2022, India recorded over 14 lakh new cancer cases. The most common among them reveal the dual challenge we face — limited screening and deep-rooted lifestyle risks.
These numbers represent every cancer type. But three cancers—breast, kidney, and prostate—illustrate the detection gap most clearly. Each shows the same pattern: early detection saves lives, late detection costs them.
The leading cancers in India reflect both screening gaps and behavioral patterns.
Top 5 Cancers by Incidence in 2022:
- Breast cancer: 192,020 cases (13.6%)
- Lip and oral cavity: 143,759 cases (10.2%)
- Cervical cancer: 127,526 cases (9.0%)
- Lung cancer: 81,748 cases (5.8%)
- Esophageal cancer: 70,637 cases (5.0%)
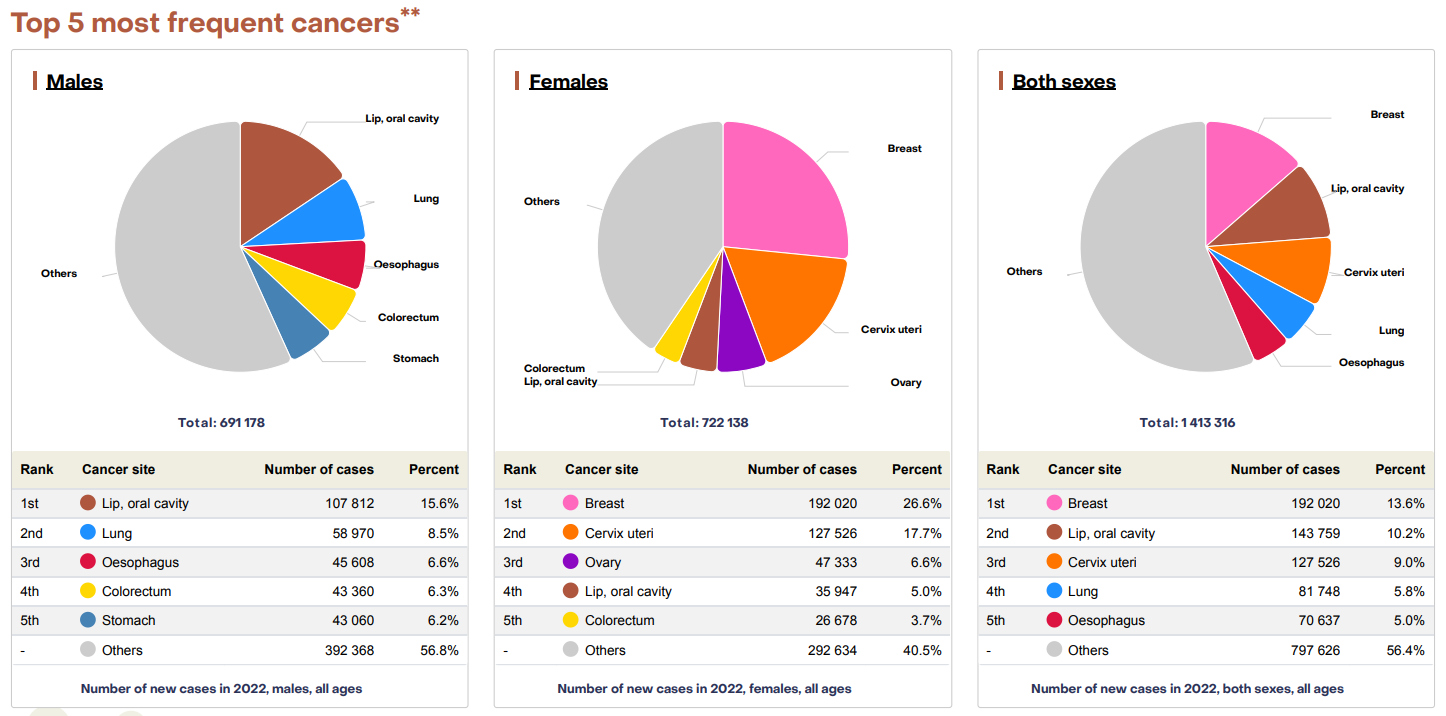
Prostate cancer, while ranking 12th overall with 37,948 cases, shows alarming growth trends. Multiple population-based cancer registries across India have recorded statistically significant increases, with annual percentage changes reaching 11.6% in some urban areas.
Let's examine three cases that reveal how detection timing shapes survival outcomes.
{{divider}}
#1: When "Probably Just a Lump" Becomes Stage 3
My friend's breast cancer journey began with what felt like a small discovery—a lump during a routine self-examination. We told ourselves the reassuring statistics: most lumps are benign. She'd schedule an appointment. It would be nothing.
But by the time diagnosis confirmed triple negative breast cancer weeks later, it was Stage 3.
The Detection Gap in Indian Breast Cancer
In India, 192,020 women were diagnosed with breast cancer in 2022—making it the most common cancer in the country. Many, like my friend, found lumps themselves, not through screening programs. By then, the cancer had already progressed.
The detection gap is significant: self-examination typically finds lumps at Stage 2-3, when tumors are large enough to feel. Clinical mammography and screening catch abnormalities at Stage 1 or even pre-cancerous stages—long before any lump is palpable.
The Survival Difference
Stage 1 breast cancer has approximately 100% five-year survival rate. Stage 3 drops to 72%. That 28-percentage-point difference represents thousands of Indian women annually whose outcomes could change with earlier detection.
For my friend, Stage 3 meant aggressive chemotherapy, longer treatment timelines, more invasive interventions, and fighting from a position of disadvantage rather than strength.
Why Women Delay Screening
Several factors contribute to late-stage breast cancer diagnosis in India:
- Cost concerns: Mammography and diagnostic tests present financial barriers
- Lack of awareness: Many women don't know recommended screening ages or frequency
- Fragmented healthcare access: Scheduling appointments, finding specialists, and navigating the system takes time
- False reassurance: The belief that "lumps are probably benign" delays medical consultation even after discovery
- Stigma and cultural factors: Discomfort discussing breast health or seeking preventive care
Breast cancer shows the detection gap for India's most common cancer. The next story shows what happens when screening isn't standard protocol—and what's possible when organizations make it so.
{{divider}}
#2: When Prevention Becomes Life-Saving: The Druva Story
Early cancer screening isn't theoretical. It delivers measurable outcomes.
Druva Data Solutions, a data security company, partnered with Loop Health to modernize its employee health benefits. Ratnadeep Ray, Druva's HR head, wanted a proactive approach that kept employees healthy rather than simply managing illness.
The first step: comprehensive Annual Health Check-ups for all employees, including advanced screening parameters and cancer markers.
During the very first round of screenings, one employee was diagnosed with Stage 1 kidney cancer.
This person had no symptoms. They felt fine. Without proactive screening, the cancer would have remained undetected until symptoms appeared—likely at Stage 3 or 4, when treatment becomes far more difficult and survival rates drop significantly.
The Detection Gap
Without routine screening programs, kidney cancer is typically found at Stage 3-4. In India, approximately 56% of kidney cancer cases are diagnosed at advanced stages. Most discoveries happen incidentally during imaging for other conditions, or after symptoms emerge—both indicators of progression.
The Survival Difference
Stage 1 kidney cancer has a 93% five-year survival rate. Stage 4 drops to 13%. The Druva employee's early diagnosis meant they could begin treatment immediately, continue contributing at work during recovery, and maintain quality of life—with 93% survival odds instead of 13%.
Why Screening Matters for Asymptomatic Cancers
Kidney cancer demonstrates a critical principle: the absence of symptoms doesn't mean the absence of disease. Cancers that grow silently require proactive screening. Waiting for warning signs means waiting for advanced disease.
Organizations that implement preventive screening catch these invisible cancers when treatment is most effective. The employee diagnosed through Druva's program represents what's possible when screening becomes standard practice rather than reactive care.
Kidney cancer demonstrates screening's power even for "invisible" cancers. The next story reveals how cultural and systemic barriers create the widest detection gap—and what India can learn from countries that screen differently.
{{divider}}
#3: Why India Catches Prostate Cancer 5× Later Than the USA
November is Movember, a global movement dedicated to men's health, particularly prostate and testicular cancer awareness. For Indian men, this focus carries special urgency.
Prostate cancer ranked 12th among all cancers in India in 2022, with 37,948 new cases and 18,386 deaths. That mortality-to-incidence ratio of nearly 50% means almost half of all diagnosed cases result in death.
The question is: why?
This ratio is significantly higher in India compared to Western countries with more established screening programs.
The Detection Gap That Costs Lives
Research shows a stark difference in how prostate cancer presents across countries:
- India: 42.9% of cases diagnosed with distant metastasis
- USA: 8.0% of cases diagnosed with distant metastasis
- Norway: 8.9% of cases diagnosed with distant metastasis
When prostate cancer is detected at Stage 1, the five-year survival rate exceeds 95%. When diagnosed at Stage 4 with distant metastasis, survival rates drop dramatically.
India's 42.9% distant metastasis rate compared to the USA's 8% isn't destiny. It's a reflection of screening culture differences that can be changed. Countries that normalize prostate screening for men over 50, make PSA testing accessible, and reduce cultural stigma catch cancer early. Countries that don't, catch it late.
The prostate cancer story shows what happens when screening gaps persist—and what's possible when they close.
{{divider}}
Why India Is Catching Prostate Cancer Late
Several factors contribute to late-stage diagnosis:
Limited Screening Culture: Lower screening practices have been observed across India, partly due to ongoing debates about PSA testing effectiveness and partly due to limited access to screening programs.
Absence of Symptoms in Early Stages: Early prostate cancers usually cause no symptoms. By the time symptoms appear—difficulty urinating, blood in urine, erectile dysfunction, bone pain—the cancer has often advanced.
Stigma: Cultural discomfort discussing prostate health causes many men to delay seeking medical attention even when symptoms emerge. The prostate-specific nature of screening tests adds another barrier to care.
Fragmented Healthcare Access: Rural areas have particularly limited access to urologists, screening facilities, and specialist care. Even in urban centers, navigating the healthcare system to arrange prostate screening requires time and resources many men don't have.
The Rising Trend
Multiple population-based cancer registries across India show statistically significant increases in prostate cancer incidence:
- Chennai: 4.4% annual percentage change
- Delhi: 3.3% annual percentage change
- Bangalore: 3.4% annual percentage change
- Kamrup Urban District: 11.6% annual percentage change
Projections using statistical models predict the age-standardized incidence rate could reach 9.15 by 2031.
What the Prostate Cancer Gap Reveals
India's 42.9% distant metastasis rate compared to the USA's 8% isn't destiny. It's a reflection of screening culture differences that can be changed. Countries that normalize prostate screening for men over 50, make PSA testing accessible, and reduce cultural stigma catch cancer early. Countries that don't, catch it late.
The prostate cancer story shows what happens when screening gaps persist—and what's possible when they close.
{{divider}}
The Common Thread: Detection Timing Determines Survival
Three different cancers. Three different detection stories. One consistent truth emerges:
In India, when cancer is detected matters more than almost anything else.
- Breast cancer found through self-examination at Stage 3: 72% survival
- Breast cancer caught through screening at Stage 1: ~100% survival
- Kidney cancer discovered after symptoms at Stage 4: 13% survival
- Kidney cancer caught through workplace screening at Stage 1: 93% survival
- Prostate cancer diagnosed after metastasis (42.9% of Indian cases): 30% survival
- Prostate cancer detected early through screening: 95%+ survival
The pattern repeats across cancer types: early detection means better treatment options, less invasive interventions, lower costs, preserved quality of life, and dramatically higher survival rates.
But early detection in India faces unique challenges. Even when screening catches cancer early, patients must navigate specialist appointment delays, fragmented care systems, treatment scheduling gaps, and financial barriers. Early detection provides the critical time buffer needed to overcome these obstacles before disease progression makes treatment more difficult.
For organizations, implementing preventive screening programs delivers measurable outcomes: lives saved, lower long-term medical costs, higher employee satisfaction, and improved retention.
For individuals, screening regularly means catching cancer at treatable stages—when survival rates are highest and treatment is least invasive.
{{divider}}
The Takeaway: Three Stories, One Lesson
Three cancer stories from 2025 tell the same tale:
Breast cancer: My friend found a lump. Diagnosed weeks later at Stage 3. Fighting an uphill battle with 72% five-year survival odds.
Kidney cancer: Druva employee had no symptoms. Screened proactively through workplace program. Diagnosed at Stage 1. Treated immediately. Life saved—93% survival odds.
Prostate cancer: Across India, 42.9% of men are diagnosed only after the cancer has metastasized to distant organs. In countries with strong screening cultures, that number is 8%.
The difference between these outcomes isn't luck, genetics, or fate. It's screening.
India recorded 1.4 million new cancer cases in 2022. Every Indian has a 10.6% lifetime risk of developing cancer before age 75. Behind each statistic is a person—someone's friend, colleague, parent, child.
This National Cancer Awareness Day and Movember, the action is clear: screen early, screen regularly, and support others in doing the same.
Early cancer screening isn't an option in India's healthcare landscape. It's essential—whether you're a woman concerned about breast cancer, a man entering Movember with prostate cancer risk, or an employee benefiting from workplace health programs.
Because cancer doesn't discriminate. But screening does. It discriminates between Stage 1 and Stage 4. Between 95% survival and 30%. Between catching cancer when it's treatable and catching it when it's not.
Between life and loss.
{{divider}}
Schedule your comprehensive health screening today. For organizations looking to implement preventive-care-first health benefits that deliver measurable outcomes—including lives saved—explore Loop Health's approach.
{{divider}}
Dedicated to everyone fighting cancer with courage and determination—especially those diagnosed this year who remind us that warriors come in many forms. Your stories inspire others to screen early and fight from a position of strength.















